Need help?
[email protected]We have learned much about COVID-19 since the pandemic began a year ago. We have new and better treatments, better patient outcomes, and better understanding of the complications and long-lasting effects of this coronavirus. New coding guidelines have been developed, with a new ICD-10 code (U07.1), and the guidelines continue to evolve.
Because the U07.1 code can substantially affect hospital reimbursement, audit contractors are paying very close attention. In this post we want to shed light on the most important factor in accurate coding and DRG assignment for COVID-19, which is the distinction between an active infection and one that is considered resolved.
Get our CDI Pocket Guide® for more help with COVID-19.
We begin with the Official Coding Guidelines, which states that only confirmed cases of COVID-19 are coded U07.1. A confirmed case is defined as having either:
1. A positive COVID-19 test result
or
2. Provider documentation that the individual has COVID-19.
This definition accounts for the fact that the standard PCR and point-of-service rapid antigen tests for COVID-19 are reliable when positive but not so much when "negative." A negative result does not rule out COVID19, because the window of time in which these tests can detect the virus is very limited (it must still be detectable in the upper respiratory tract). These false negative rates range from 20% to 60% depending on whether the patient has symptoms. Therefore, the provider can make a clinical decision whether the patient has COVID-19 infection, even if the test is negative or no test was performed.
Hospitals are reimbursed for COVID-19 patients based on the assignment of ICD-10 code U07.1 on a claim. The hospital also earns an extra 20% bonus from CMS to cover the unusual costs of treating and isolating an infectious patient in a pandemic.
If U07.1 is coded as the principal diagnosis, the following DRGs might be assigned: DRG 177-179 (Respiratory Infections), DRGs 207-208 (with ventilator), and sometimes DRGs 981-983/987-989 if an OR procedure is performed.
If code U07.1 is assigned as a secondary diagnosis, it is classified as an MCC—even if the patient is asymptomatic.
Because testing strategies have evolved, and a 20% bonus is something payers will not eagerly part with, the rules changed as of September 1, 2020. Now, to qualify for the 20% reimbursement bonus, the record must contain a positive COVID-19 test (either during the admission or within 14 days prior to admission). If the record does not contain the positive test report, hospitals can decline the additional payment at the time of claim submission to avoid repayment.
According to current coding guidelines, code U07.1 can be assigned for patients admitted with a positive COVID test or manifesting an active infection.
Patients readmitted with complications or residual effects of a previous COVID-19 infection are not coded with U07.1, because their infection is considered to be inactive or have "resolved." Symptoms can linger, evolve, or rebound, but these do not prove that the virus is still active or infectious.
In short, we can't know for sure, but there are guidelines.
The CDC states that “Available data indicate that persons with mild to moderate COVID-19 remain infectious no longer than 10 days after symptom onset. Persons with more severe to critical illness or severe immunocompromise likely remain infectious no longer than 20 days after symptom onset; however, there have been several reports of people shedding replication-competent virus beyond 20 days due to severe immunocompromise."
So, if the patient has mild to moderate COVID-19, they're considered resolved after 10 days from onset.
If the patient has severe or critical illness, or is immunocompromised, the infection may be active up to 20 days from onset.
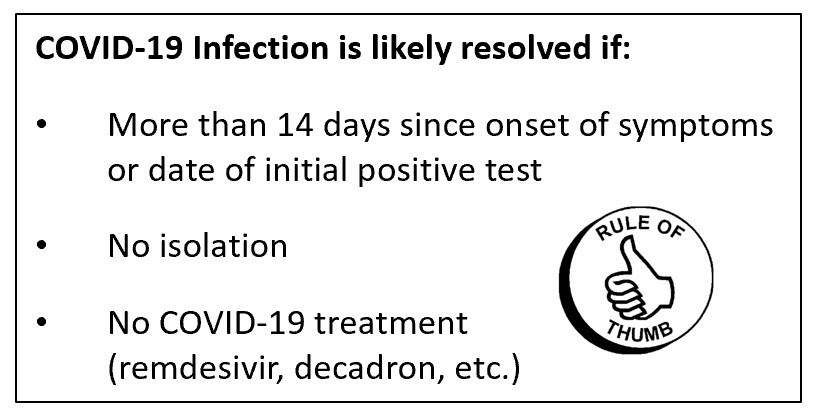
There are also clinical clues that an infection has resolved: the patient isn't isolated, and there is no COVID-19 treatment being given (remdesivir, decadron/dexamethasone, etc.).
Although a repeat test may be useful in patients with new symptoms, retesting is not generally recommended, because patients who have recovered from a COVID-19 infection may continue to shed viral RNA or dead virus may continue to circulate in the body. True reinfection is uncommon. Therefore, the CDC advises that providers not repeat COVID tests following an initial positive test.
Whether or not COVID-19 is assigned as the principal diagnosis is dependent on whether the COVID-19 infection has resolved which is determined by provider documentation. If a patient is admitted with a residual effect (sequelae) and the provider documentation indicates the COVID-19 infection has resolved or the patient is no longer infectious (even with a current or recent positive COVID-19 test), assign a code for the residual effect as principal diagnosis and code U09.9, Post-COVID-19 condition. If the COVID-19 infection has not resolved, assign code U07.1 as principal diagnosis and the manifestation as a secondary diagnosis.
Coding Clinic 2021 Fourth Quarter has clarified that even if a patient has a current or recent positive test for COVID-19, when provider documentation indicates that a patient is not actively infectious during the admission, this indicates that the patient no longer has an active COVID-19 infection, and code U07.1 would not be assigned. See FAQ pages 21-24, Questions #53, 55-58.
Considering the CDC data and the CMS requirement for a positive test within the past 14 days, a good rule of thumb is that if it's been more than 14 days since a patient had onset of mild or moderate symptoms, or more than 20 days in a severely ill patient, then the infection is likely to have resolved.
Based on official coding guidelines and the ICD-10-CM instructions for COVID-19, the following are six clinical and coding scenarios to help guide you in coding and sequencing code U07.1.
Case 1. Patient admitted with pneumonia and respiratory failure. Patient tested positive for COVID-19 infection 10 days ago.
Here, Code U07.1 is assigned as the principal diagnosis, with the respiratory manifestations as secondary diagnoses. According to Coding Clinic, providers do not have to explicitly link the respiratory manifestation with COVID-19 since the causal relationship is implied. Common respiratory manifestations include pneumonia, lower respiratory infection, pneumothorax, acute respiratory failure, and ARDS. The test report should be accessed and included in the admission record.
Case 2. A patient was diagnosed with COVID-19 infection a week ago and is admitted after developing acute shortness of breath associated with upper back pain as well as dizziness, fever and cough. The patient was discharged with the diagnosis of pulmonary embolism (PE) due to COVID-19 infection.
When the reason for the admission is a non-respiratory manifestation of COVID-19, code U07.1 is assigned as the principal diagnosis and the manifestation(s) as secondary. In applying this rule, the provider must specifically “link” COVID and a non-respiratory manifestation. Common non-respiratory manifestations include thrombo-embolism resulting in CVA, MI, DVT, pulmonary embolism; COVID-related enteritis, multisystem inflammatory syndrome in children (MIS-C), cytokine release syndrome, and Guillain-Barré syndrome. Here, pulmonary embolism is assigned as a secondary diagnosis.
Case 3. Patient was admitted with COVID-19 pneumonia three weeks ago, and is now being readmitted for a pulmonary embolism.
This is a great example of coding the sequelae of COVID-19. A sequela is a manifestation or complication of a previous condition (sequelae is the plural). When a patient is admitted with sequela of a prior COVID-19 infection, code the sequela as the principal diagnosis with a secondary diagnosis code of U09.9, Post-COVID condition. Some common sequelae include pneumonia, cytokine release syndrome, thromboembolism resulting in CVA, MI, DVT or PE and heart failure (for those who had COVID myocarditis).
In this case, since it's been three weeks since the last admission (and therefore > 14 days since symptom onset), we would assign pulmonary embolism as the principal diagnosis, and U09.9 as a secondary diagnosis.
Case 4. Elderly patient was admitted for hip fracture s/p fall at home. Patient has weakness and generalized debility due to prolonged hospitalization one month ago for COVID-19.
Here the patient has a hip fracture, which is not directly related to the previous COVID-19 infection, which has resolved by now. We would assign the unrelated condition (hip fracture) as the principal diagnosis and assign code Z86.16 (Personal history of COVID-19) as a secondary diagnosis. Personal history codes account for a patient's past medical condition that no longer exists and is not being treated but may recur. According to Coding Clinic, code U09.9 (sequelae) would not be assigned, as the debility is due to the prolonged hospitalization rather than COVID-19 infection itself.
Case 5. Patient admitted with severe anemia due to chronic GI bleeding. Also experienced low-grade fever and mild shortness of breath, which led the hospital to test for COVID-19. The patient tested positive, was placed in isolation, and treated with blood transfusions.
When an admitted patient has COVID-19 and an unrelated condition, sequencing depends on which diagnosis meets the definition of the principal diagnosis. When two or more diagnoses "equally meet the criteria for principal diagnosis as determined by the circumstances of admission, diagnostic workup, and/or therapy provided ….any one of the diagnoses may be sequenced first.”
The circumstances in this case favor anemia as the focus of admission, particularly since COVID-19 in this case was not severe enough to require admission on its own. Assign anemia as principal diagnosis and COVID-19 (U07.1) as secondary diagnosis.
Special cases: Sepsis, Transplant Complications, and Obstetrics
In these special cases, code U07.1 follows the required principal diagnosis definition based on Official Coding Guidelines:
Case 6. Patient is admitted with COVID pneumonia and sepsis. Whether or not sepsis or U07.1 is assigned as the principal diagnosis depends on the circumstances of admission and whether sepsis meets the definition of principal diagnosis. For example, if a patient is admitted with pneumonia due to COVID-19 which then progresses to viral sepsis (not present on admission), the principal diagnosis is U07.1, COVID-19, followed by the codes for the viral sepsis and viral pneumonia. On the other hand, if a patient is admitted with sepsis due to COVID-19 pneumonia and sepsis meets the definition of principal diagnosis, then the code for viral sepsis (A41.89) would be assigned as principal diagnosis followed by codes U07.1 and J12.82, as secondary diagnoses. In most cases, the principal reason for admission and focus of treatment is the COVID-19 pneumonia and its consequences, with U07.1 assigned as the principal diagnosis.
Case 7. Patient is status post lung transplant, admitted with pneumonia and COVID-19. The transplant complication code (T86.812) is assigned as principal diagnosis since the pneumonia is affecting the function of the transplanted organ.
Case 8. A patient who is 30 weeks pregnant is admitted with COVID-19. Code O98.5 (Other viral diseases complicating pregnancy, childbirth and the puerperium), is assigned as the principal diagnosis and code U07.1 with the associated manifestation(s) are secondary diagnoses.
Physicians and other healthcare staff are overwhelmed with high caseloads of very sick COVID-19 patients. Therefore, although hospitals should use code U07.1 when it is appropriate, we also want to minimize COVID-19 queries.
CDI and coding specialists should consider the above “rule of thumb” when patients are admitted with a previous COVID-19 infection (“history of,” “convalesced,” "resolved”). In many of these situations, no query would be needed and code U07.1 would not be assigned—even if the patient continues to test positive.
If there are indicators of a current, active infection, such as 14 days or less since COVID-19 infection (or positive test), treatment with medications for COVID-19 (dexamethasone, remdesivir, etc.), or the patient is placed in isolation, then a query would likely be productive if the documentation is unclear.
Other situations when a query may be needed is when provider documentation is unclear whether a non-respiratory condition is related to a current COVID-19 infection. Clinical validation comes into play when clinical indicators are questionable and test results are negative or absent; pay attention to the combination of duration since symptom onset and severity of symptoms—remember, severe cases or people who are immunocompromised may have active infections up to 20 days from onset, rather than 10 days for less severe cases.
Updated 02/07/2022 with new ICD-10 codes.
Receive updates on new Resources, Products, and Events.
