Need help?
[email protected]Coagulation disorders are disorders of the blood clotting factors that disrupt the body's ability to control blood clotting, resulting in either abnormal bleeding or excessive blood clotting. Either can be hereditary or acquired. The general terms “hypo-coagulopathy” is defined as an increased tendency toward bleeding and “hyper-coagulopathy” as an increased tendency toward blood clotting (thrombosis), respectively.
In this article, we will focus on the hypocoagulopathies, i.e., coagulation disorders causing hemorrhage.
There are 12 blood clotting factors, Factors I-V and VII-XIII. All the blood clotting factors are produced by the liver, except Factor IV. Vitamin K is needed for the liver to produce Factors II, VII, IX, X. Phospholipids are components of the cellular and platelet membranes and provide a surface for the chemical reactions of coagulation to take place.
What can disrupt the coagulation process? Many things can, including:
Hereditary hypocoagulopathy, or hemophilias, are very rare and include Von Willebrand disease (VW factor deficiency or abnormality), Hemophilia A (clotting Factor VIII deficiency) and Hemophilia B (clotting Factor IX deficiency.
Acquired hypocoagulopathies are common and usually due to drugs that interfere with normal clotting factors, such as anticoagulants like Coumadin and Eliquis, or antithrombotic drugs that interfere with platelet function like aspirin or Plavix. Severe liver disease causes decreased production of clotting factors, and autoimmune diseases may be associated with inhibitors of clotting factors, e.g., lupus anticoagulant or antiphospholipid antibodies.
Get our CDI Pocket Guide® for more help with identifying coagulation disorders.
Prothrombin time (PT). Prothrombin is a crucial clotting factor made by the liver. The prothrombin time (PT) is a test that measures how long it takes for a clot to form in a blood sample. The international normalized ratio (INR() is a standardized calculation based on the PT. The PT/INR determines if the blood is clotting normally and measures the therapeutic effectiveness of Coumadin for patients with atrial fibrillation, thromboembolism, stroke, etc. An elevated INR may represent a therapeutic effect or adverse reaction when it causes bleeding.
Below are the INR values and what these indicate:
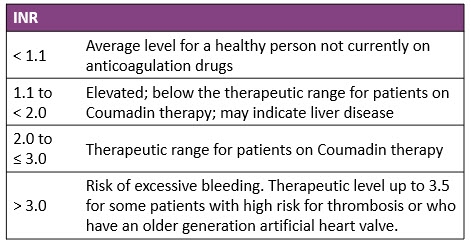
Other reasons for a high INR include inherited or acquired clotting factor deficiency (I, II, V, VII, X), DIC, Vitamin K deficiency and liver disease.
Partial thromboplastin time (PTT). The partial thromboplastin time (PTT) is the time in seconds it takes plasma to clot and measures a different set of clotting factors than the PT. The normal range is 60-70 seconds. Activated PTT (aPTT) is the same test as PTT, but an activator is added that speeds up the clotting time and test results. The normal range is 30-40 seconds. PTT/aPTT are also used to measure the effectiveness of heparin therapy. Patients on Heparin should have a PTT or aPTT 2 to 2.5 times the normal range.
These laboratory findings may indicate:
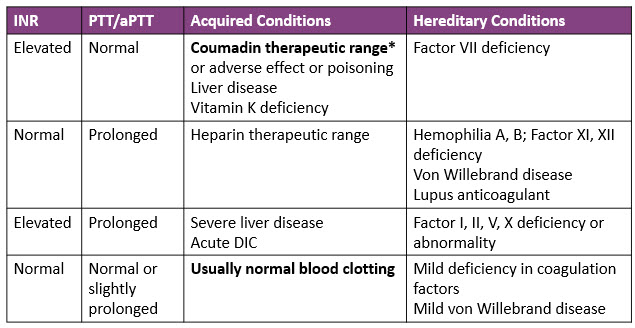
*For patients on Coumadin therapy: Expected therapeutic range for INR is 2.0 to 3.0. For some patients who have a high risk for thrombosis, the INR needs to be higher: 2.5 to 3.5.
For patients who are presurgical: Coumadin is held and INR/PTT should be ≤ 1.5 (there are some exceptions where it must be normal) to reduce the risk of bleeding. Patients not on Coumadin: INR should be normal (<1.1) or cause investigated.
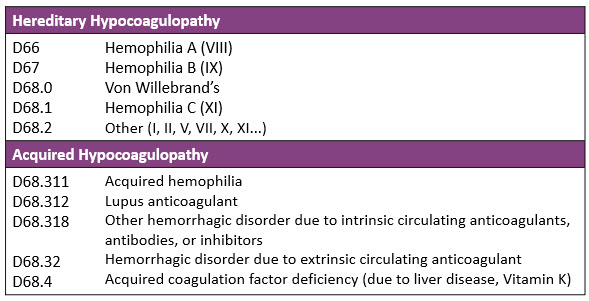
Other ICD-10 codes that are not coagulation disorders include:
R79.1, Abnormal coagulation profile: This code should be assigned for patients on anticoagulant therapy, and the PT/INR is elevated, but not causing bleeding.
Z79.01 Long term use (current) of anticoagulants: This code should be assigned for patients on anticoagulant therapy, and the PT/INR is in therapeutic range.
Principal Diagnosis Sequencing: When an anticoagulant or antithrombotic causes the adverse reaction of bleeding, sequencing of D68.32, Hemorrhagic disorder due to extrinsic circulating anticoagulants, and the cause/site of bleeding depends on the circumstances of admission. Was the “focus” of the admission the bleeding itself (e.g., evaluation, procedures, transfusion, monitoring, H/H) or the correction of the bleeding disorder (e.g., vitamin K, fresh frozen plasm)?
Case 1. Patient with epistaxis and taking Coumadin as prescribed; nosebleed treated with nasal packing. Admitted with INR 6.8, treated with fresh frozen plasma to reverse elevated INR, discontinuation of Coumadin, serial hemoglobin and INR, and subsequent cautious resumption of Coumadin based on INR.
Here the principal diagnosis is D68.32, Hemorrhagic disorder due to extrinsic circulating anticoagulants [if documented]. Secondary diagnoses include T45.515A, Adverse effect of anticoagulants, and R04.0, Epistaxis. The hemorrhagic disorder was the focus of the admission and an adverse effect of Coumadin.
If Coumadin was taken improperly, i.e., poisoning, the poisoning code (T45.511- or T45.521) would be sequenced first.
Case 2. Patient admitted with GI bleeding while properly taking Plavix. Treatment included discontinuation of Plavix, blood transfusion, EGD and colonoscopy, which was identified a bleeding gastric ulcer.
The principal diagnosis in this case is K25.4, Gastric ulcer with bleeding. Secondary diagnoses include D68.32, Hemorrhagic disorder due to extrinsic circulating anticoagulants [if documented], and T45.525A, adverse effect of antithrombotic. The ulcer with bleeding was the focus of the admission and an adverse effect of Plavix (antithrombotic).
Cases 3 to 5: Surgical patient
Case 3. 52-year-old female, morbidly obese, admitted for exploratory lap, abdominal hysterectomy/BSO for uterine fibroids on Oct. 26. Patient was noted to have considerable post-operative incisional bleeding due to subcutaneous hematoma, return to OR for wound exploration and closure.
Pt on Coumadin held for surgery and Lovenox given. Labs 10/26: PT 18.3/INR 1.61.
This clinically indicates: D68.32, Hemorrhagic disorder due to extrinsic circulating anticoagulants.
Case 4. 52-year-old female, morbidly obese, admitted for exploratory lap, abdominal hysterectomy/BSO for uterine fibroids on Oct. 26 without complication.
Pt on Coumadin held for surgery and Lovenox given. Labs 10/26: PT 18.3/INR 1.61. PN: Elevated PT/INR.
An abnormal PT/INR or PTT due to an anticoagulant that does not cause bleeding is assigned code R79.1, Abnormal coagulation profile.
Case 5. 52-year-old female, morbidly obese, admitted for exploratory lap, abdominal hysterectomy/ BSO for uterine fibroids on 10/26 without complication.
Pt on Coumadin held for surgery and Lovenox given; INR 1.1.
The PT/INR is in the therapeutic range. Assign code Z79.01, Long term (current) use of anticoagulants.
© 2022 Copyright Pinson & Tang
Receive updates on new Resources, Products, and Events.
